Design Verification Testing of Combination Products
A Primer on the Roadmap for Developing an Injectable Combination Product
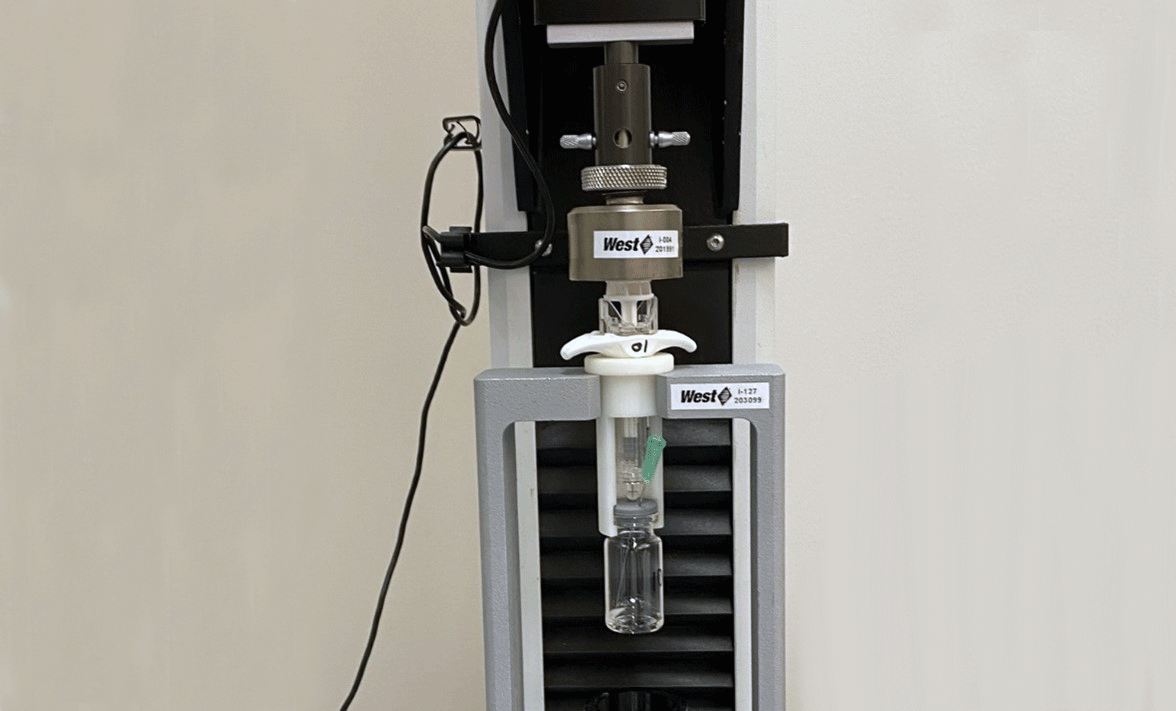
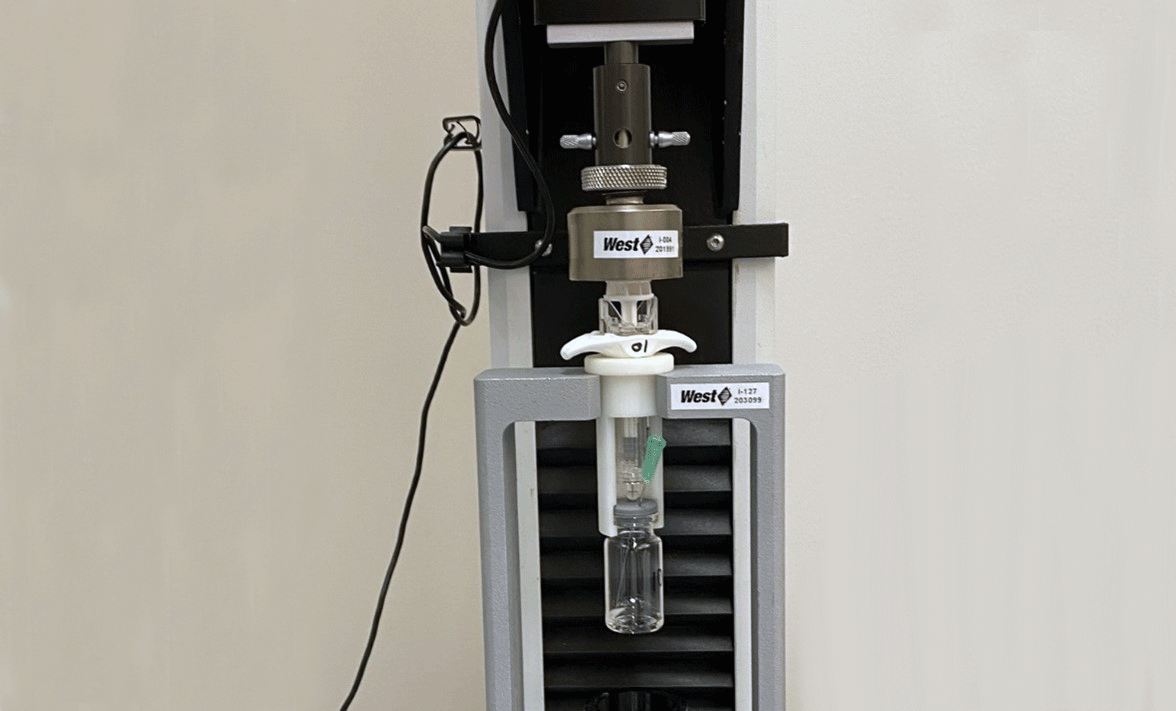
West's analytical laboratoryi performs many services for combination products, including Design Verification Testing (DVT). This testing is not only performed for West’s contract manufacturing clients or for pharma partners that use West’s self-injection devices but also as a service offering to clients who may be developing combination products with non-West device constituents. Clients often come to West saying that they are developing a particular combination product, like a pre-filled syringe or an auto-injector, and ask for a list of tests that they need to have performed in order to complete DVT. The answer to that question is more complex than picking tests off of a standard list. The tests for each combination product must be derived from holistic Risk Assessment processes, with considerations for both drug and device. On the device side, the list of tests will be reflected in the Design Inputs. Even for a generic or biosimilar product, while one can use the innovator’s product as a guide, the Design Inputs, and the Design Verification tests that come out of it, must be derived and justified.
According to 21 CFR part 4,ii the federal regulation for combination products, drug-led combination products must follow pharmaceutical current good manufacturing practices found in 21 CFR parts 210iii and 211iv as well as select sections of 21 CFR part 820,v including having a device Quality Management System (21 CFR part 820.20) in place and following Design Controls (21 CFR part 820.30).
Planning
The starting point for realizing a combination product is to author a Design and Development Plan. This plan outlines all of the planned activities, project stages, project review points and the milestones that must be met to progress to each subsequent project stage. Furthermore, the plan assigns responsibilities and resources for specific tasks to ensure that all involved functions (Engineering, Quality, Supply Chain, Manufacturing, etc.) understand what efforts they need to contribute towards the project’s success. The Design and Development Plan is intended to be a living document that is updated as new information and developments become available. Whether the product is an innovative combination product or a generic version of an existing product, the same steps must be followed in development. This plan becomes a part of the Design History File for the combination product and demonstrates to regulatory bodies that the combination product was properly planned and developed and not haphazardly thrown together.
Design Inputs
Before any design work is performed, it is critical to establish Design Inputs which must address all the biocompatibility, functional, performance, usability, reliability, safety, storage and distribution requirements of the intended combination product. These requirements should be based on appropriate Standards, regulatory guidance documents, known human factors data relevant to the user population, formative human factors studies and, of course, Risk Assessments, as described in ICH Q9,vi AAMI TIR 105:2020vii and ISO 14971:2019.viii For example, if an auto-injector based combination product is being designed, it is important to consider requirements outlined in ISO 11608-5:2022.ix In addition, one needs to consider the users who might be operating that auto-injector based combination product and match their needs and abilitiesx in setting the Design Inputs. If the intended users have dexterity issues, due to arthritis or other conditions, then the design specifications need to be tailored to their capabilities to assure regimen adherence. Design Inputs must also include the acceptance criteria for future device testing, based on the needs of the user and the planned device.
Risk assessments should consider what happens when the user attempts to administer the drug with the combination product but they should also consider the manufacturing of the components, the assembly of the device, the compatibility of the materials with the drug, the fill/finish process and the transportation and storage of the combination product. Risk Assessments can be conducted using a number of different methodologiesxi but the most common are the Failure Mode Effects Analysis (FMEA), the Ishikawa (fishbone) diagram and the Fault Tree Analysis.
The output from the risk assessment is a list of Critical Quality Attributes (CQAs). These are defined in ICH Q8xii as “physical, chemical, biological, or microbiological properties or characteristics that should be within an appropriate limit, range, or distribution to ensure the desired product quality.” While technically these apply to pharmaceutical development, it can also be helpful to consider them as Design Inputs for drug led combination product development. In fact, the FDA guidance documentxiii on ICH Q8 does refer to its applicability to dosing devices such as dropper pipettes, pen injection devices and dry powder inhalers, all parts of drug-led combination products. CQAs are identified based on the severity of harm, as far as the safety and efficacy of the treatment, that can result if these attributes are not met. For example, if it is known that the combination product user population has limited strength in their hands due to their health conditions, the Break Loose and Extrusion forces for a self-administered pre-filled syringe must be below a certain level or else the user would not be able to administer the product. The Break Loose and Extrusion forces are CQAs for that combination product.
Part of the evaluation of risk is a determination of whether the product meets the required reliability level. A high-risk failure mode usually requires a 99% reliability to assure that the failure does not occur more than 1% of the time. A medium-risk failure mode usually requires a 97.5% reliability while a low-risk is acceptable at 95% reliability (sometimes those reliability values are chosen to be 99%, 95% and 90%, respectively). The reliability requirements of the combination product determine the sample sizes required for Design Verification Testing (DVT). More details on sample sizes for DVT can be found in ISO 11608-1:2022 Annex F.xiv
Essential Performance Requirements (EPRs) are Critical Quality Attributes of the combination product that impact patient safety or clinical performance at the time of use by the patient or user. These can be thought of as Essential Outputs from Design Controls, 21 CFR 820.30(d), which mandates that “design outputs that are essential for the proper functioning of the device are identified.” Once established, EPRs become a subset of Established Conditions (described in ICH Q12xv) that are “necessary to assure product quality” as the elements of the Control Strategy (described in ICH Q10xvi) and can only be changed with prior approval from regulatory agencies. EPRs are also typically evaluated in drug-device release testing and during stability studies to demonstrate that the combination products perform as intended, unless the underlying performance of the EPR can be evaluated upstream of the final release, thus avoiding retesting at release.xvii
Design Outputs
Once the specifications are set, the design process can begin, and this process may require several iterations until the desired product is realized. This involves evaluating device designs, components, suppliers, material compatibility, manufacturing processes, etc. The Design Outputs that result from the design iterations include drawings, selected components and suppliers, manufacturing documentation and other Established Conditions that lock-in the characteristics of the product and ensure that the resulting device would perform as intended. In addition, the instructions-for-use, product packaging and labelling need to be established. The Design Output evaluation will include some performance testing to determine whether the Design Input performance requirements are being met or if additional design iterations are required.
Design Verification
Once the product design has been finalized, Design Verification can take place to provide objective evidence through measurable means that the Design Outputs from the final product design meet the Design Input requirements. This is typically performed through laboratory testing, where the performance of the product design is evaluated. The testing is performed with validated methods,xviii using statistically justified sample sizes and with set acceptance criteria. Often, samples are tested which have been stored at label storage conditions as well as conditions appropriate to simulate accelerated aging, thermal conditioning and transportation conditioningxix to demonstrate the robustness of the product design.
Once the design has been verified, Design Validation must be carried out to demonstrate that the product design meets the needs of the intended use. This is usually performed through a clinical evaluation with actual or simulated users and utilizes representative product to ensure that the results of the studies reflect real world expectations.
For a more detailed discussion of injectable combination product development, please see the review article published by Fran DeGrazio and Diane Paskiet.xx
- West's analytical laboratories are part of West Services and Solutions, LLC, a wholly-owned subsidiary of West Pharmaceutical Services, Inc
- Title 21 —Food and Drugs; Chapter I —Food and Drug Administration, Department of Health and Human Services, Subchapter A—General, Part 4—Regulation of Combination Products. Available at: https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-4
- Title 21 —Food and Drugs; Chapter I —Food and Drug Administration, Department of Health and Human Services, Subchapter C—General, Part 210—Current good manufacturing practice in manufacturing, processing, packing, or holding of drugs; general. Available at: https://www.ecfr.gov/current/title-21/chapter-I/subchapter-C/part-210
- Title 21 —Food and Drugs; Chapter I —Food and Drug Administration, Department of Health and Human Services, Subchapter C—General, Part 211—Current good manufacturing practice for finished pharmaceuticals. Available at: https://www.ecfr.gov/current/title-21/chapter-I/subchapter-C/part-211
- Title 21 —Food and Drugs; Chapter I —Food and Drug Administration, Department of Health and Human Services, Subchapter H—Medical Devices, Part 820—Quality System Regulation, Subpart C—Design Controls. Available at: https://www.ecfr.gov/current/title-21/chapter-I/subchapter-H/part-820/subpart-C/section-820.30
- ICH. Quality Risk Management. ICH Q9. November 9, 2005. Available at: https://database.ich.org/sites/default/files/Q9%20Guideline.pdf
- Association for the Advancement of Medical Instrumentation. Risk Management Guidance For Combination Products. AAMI TIR105:2020. Arlington, VA: AAMI, 2020. Available at: https://array.aami.org/doi/book/10.2345/9781570207709
- International Organization for Standardization. (2019). Medical devices – Application of risk management to medical devices (ISO Standard No. 14971:2019). Available at: https://www.iso.org/standard/72704.html
- International Organization for Standardization. (2022). Needle-based injection systems for medical use — Requirements and test methods — Part 5: Automated functions (ISO Standard No. 11608-5:2022). Available at: https://www.iso.org/standard/76627.html
- ANSI/AAMI HE75:2009 (R2018) Human Factors Engineering - Design Of Medical Devices. Available at: https://webstore.ansi.org/standards/aami/ansiaamihe752009r2018
- Q9(R1) Quality Risk Management. Guidance for Industry and Food and Drug Administration Staff, May 2023. Available at: https://www.fda.gov/media/167721/download
- ICH. Pharmaceutical Development. ICH Q8(R2). August 2009. Available at: https://database.ich.org/sites/default/files/Q8_R2_Guideline.pdf
- Q8(R2) Pharmaceutical Development Guidance for Industry and Food and Drug Administration Staff, Nov. 2009. Available at: https://www.fda.gov/media/71535/download
- International Organization for Standardization. (2022). Needle-based injection systems for medical use — Requirements and test methods — Part 1: Needle-based injection systems (ISO Standard No. 11608-1:2022). Available at: https://www.iso.org/standard/70733.html
- ICH. Technical and Regulatory Considerations for Pharmaceutical Product Lifecycle Management. ICH Q12. November 20, 2019. Available at: https://database.ich.org/sites/default/files/Q12_Guideline_Step4_2019_1119.pdf
- ICH. Pharmaceutical Quality System. ICH Q10. June 4, 2008. Available at: https://database.ich.org/sites/default/files/Q10%20Guideline.pdf
- Roan, S. Refining control strategy for pre-filled pen. International Pharmaceutical Quality. March-April 2018; 10(2): 36-40. Available at: https://ipqpubs.com/wp-content/uploads/2018/06/2018_march.april.v1.pdf
- International Organization for Standardization. (2015). Prefilled Syringes - Part 4: Glass barrels for injectables and sterilized subassembled syringes ready for filling. (ISO Standard No. 11040-4:2015). Section 4.2: Testing. Available at: https://www.iso.org/standard/58079.html
- ASTM Standard D4169, 2022, " Standard Practice for Performance Testing of Shipping Containers and Systems," ASTM International, West Conshohocken, PA, 2022.
- DeGrazio, F., Paskiet, D. Injectable Combination Product Development: Facilitating Risk-Based Assessments for Efficiency and Patient Centric Outcomes. J. Pharm. Sci. 2020; 109: 2101-2115. Available at: https://jpharmsci.org/article/S0022-3549(20)30179-9/fulltext