USP <382>: Think Systems, Not Components – Testing Drug Packaging and Delivery Systems – What You Need To Do
The United States Pharmacopeia (USP) requirements for elastomeric components of container closure systems used for parenteral products are changing. The scope of USP <382> Elastomeric Component Functional Suitability in Parenteral Product Packaging/Delivery Systemsi introduces a paradigm shift away from testing elastomeric components individually by the supplier, as was done historically under USP <381> Elastomeric Components in Injectable Pharmaceutical Production Packaging/Delivery Systemsii, to a holistic evaluation of these components when assembled into drug product packaging and delivery systems. In addition, the testing is performed on the final packaging/delivery system as produced by the drug manufacturer, using product-filled systems or systems filled with a suitable proxy, where applicable. As such, the elastomeric component supplier cannot perform USP <382> testing without knowledge of the specific drug product/proxy or the complete packaging system that the drug manufacturer plans to use. Therefore, the responsibility for USP <382> testing shifts from the elastomeric component supplier to the drug manufacturer.

This new chapter incorporates container closure integrity testing and an update to the functionality tests for elastomers, such that the functionality testing portion of USP <381> will soon be omitted, while the physicochemical tests for elastomer characterization described in USP <381> will remain in effect. USP <382> will become effective on December 1, 2025, allowing five years from the date of publication in December of 2020 for stakeholders to implement the new testing requirements for full compliance.
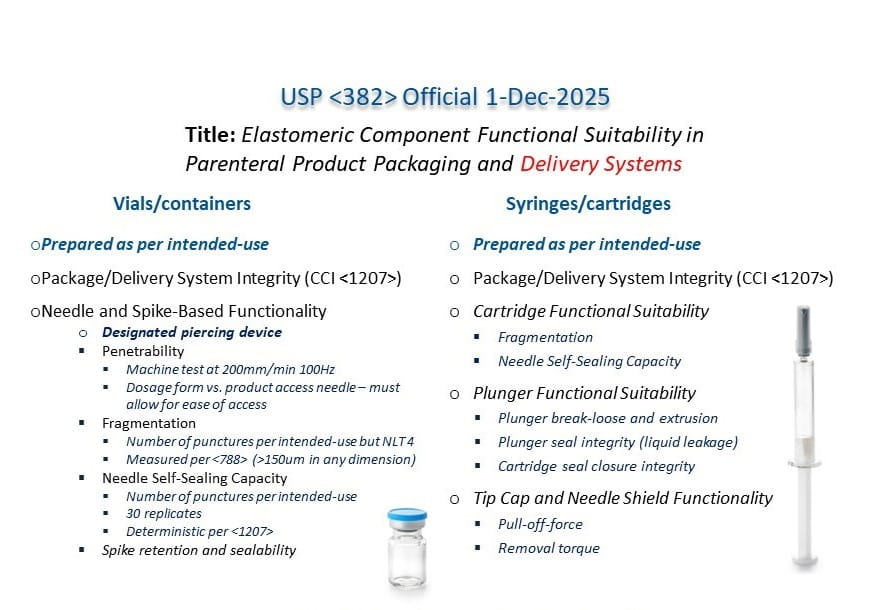 Figure 1 - Summary chart of USP <382> tests for vials, syringes and cartridges.
Figure 1 - Summary chart of USP <382> tests for vials, syringes and cartridges.
The USP chapter prescribes specific testing (partly summarized in Figure 1) to be performed for the packaging/delivery system. West has written other blogs about these tests, including fragmentation, penetration and sealability of stoppers, vial system integrity and needle sealing capacity, cartridge and syringe functional performance and syringe/cartridge system integrity. These tests are to be used as a starting point and the chapter warns that, “[t]he tests provided in this chapter are not exhaustive. Additional tests may be required to adequately assess the functional suitability of a given packaging/delivery system for a particular product.” The chapter further states that functional suitability assessment studies for each specific drug product in its final drug packaging/delivery system should be developed based on a) the system design/mechanics, b) the nature of the dosage form, c) the environment and clinical use setting of the finished drug product and d) the assessed safety of those using and/or exposed to the drug during administration, all with justification. In other words, the USP instructs the drug manufacturer to perform a risk assessment on their packaging to determine the best test strategy for the given application.
The risk assessments that one would perform to establish the design inputs in the design and development plan (21 CFR 830.30iii and ISO 13485iv ) for combination products and the risk assessments that one would perform for drugs and biologics, per ICH Q9v, should lead to the same tests described in USP <382> as well as any additional tests that USP <382> alludes to when it states that the specified list of tests is not exhaustive.
Furthermore, each of the tests described in USP <382> is informed by an ISO standard and, on the topics of container-closure integrity and fragmentation, also references those applicable USP chapters, as shown in Table 1. This alignment with the ISO standards and USP chapters is further discussed in USP <1382>vi. By aligning with applicable ISO standards, USP <382> is additionally tying the chapter’s requirements to standards that one would already be considering when developing a combination product design verification plan; or evaluating drug container compliance per 21 CFR 211.94 Drug product containers and closuresvii and per ICH Q9.
Table 1 - USP <382> tests referencing ISO documents and USP chapters.
| System | Elastomer Component(s) | USP Test
Section | Piercing
Device | ISO
Informed | USP
Reference |
|---|
| Vial/Bottle | Closure with seal | 4, 5.1, 5.2, 5.3, 5.4 | Hypodermic Needle or Spike | 8362-2, 8362-5, 8536-2, 8536-6, 8871-5 | USP <1207>
USP <788> |
| Blow-Fill-Seal | Liner in plastic cap | 4, 5.1, 5.2, 5.3, 5.4 | Spike | 15759 | USP <1207>
USP <788> |
| Plastic (Film Bag) | Septum in access port | 4, 5.2, 5.3, 5.4 | Narrow gauge Cannula or Spike | 15747, 8536-4 | USP <1207> |
| Cartridge | Plunger/Septum | 4, 5.1, 5.3, 6.1, 6.2 | Needle | 11040-2, 11040-3, 13926-2, 13926-3, 11608-3 | USP <1207>
USP <788> |
| Prefilled Syringe | Plunger/Needle-Shield/Tip-Cap | 4, 6.1, 6.2, 7 | Not applicable | 11040-4, 11040-8 | USP <1207> |
| Single-Use Syringe as Combination Product | Plunger | 4, 6.1, 6.2 | Not applicable | 7886-1, 7886-2, 7886-3, 7886-4, 8537 | USP <1207> |
This alignment of USP <382> with the USP and ISO standards that are already being used to demonstrate the suitability of drug product packaging and delivery systems begs the question of whether additional effort is required to comply with this new chapter. As is standard practice in the pharmaceutical industry, manufacturers should first complete a gap analysis between their existing studies and the requirements in USP <382>. Once the gaps are identified, risk assessment processes should guide the appropriate testing plans to close any identified gaps based on potential failure modes and patient safety.
Keep in mind that one’s testing does not have to exactly match the methods described in USP <382>. The introduction of the chapter concludes with the following paragraph:
Alternative testing strategies for functional suitability assessment may be appropriate in certain circumstances with justification. In all cases, when reporting functional suitability assessment findings, the drug product applicant is advised to offer justification for the testing program chosen.
Alternative testing strategies can be used to meet the requirements of USP <382> as long as the alternative methods are equivalent. The criteria for method equivalence are detailed in USP General Notice 6.30viii, which states:
An alternative method or procedure is defined as any method or procedure other than the compendial method or procedure for the article in question. The alternative method or procedure must be fully validated (see Validation of Compendial Procedures ⟨1225⟩) and must produce comparable results to the compendial method or procedure within allowable limits established on a case-by-case basis. Alternative methods or procedures can be developed for any one of a number of reasons not limited to simplification of sample preparation, enhanced precision and accuracy, improved (shortened) run time, or being better suited to automation than the compendial method or procedure. Only those results obtained by the methods and procedures given in the compendia are conclusive.
Another question that can arise is regarding the applicability of USP <382> to products already on the market when the chapter becomes effective on December 1, 2025. Is the chapter only applicable to new products or does it also apply to the existing approved products? Again, the introduction section reads:
Reevaluation of the functional suitability of a commercialized product’s packaging/delivery system may be required over the product’s life cycle when changes in components, processes, or the product itself occur.
The implication is that one only needs to evaluate already commercialized products when making changes to components, processes or the product itself. However, all products including previously approved products, changed products, and brand new products must comply with USP <382> requirements once the chapter becomes official. Because USP <382> is aligned with the ISO standards detailed in USP <1382> (Table 1), one could argue that data previously generated per those ISO standards is also compliant with USP <382>. If the testing strategy used in the original filing utilized a risk and science based approach and considered all applicable scenarios, even if the strategy differs from that prescribed in USP <382>, presuming that difference can be justified, then re-performing testing prescribed in the chapter may not be necessary to comply with USP <382> requirements. One point to keep in mind is that USP <382> requires using product or proxy for performance testing while ISO standards may allow for the use of water in their testing. While water may be fine for testing fragmentation, product or proxy should be used for leakage tests or break-loose and extrusion tests because the properties of the product or proxy could affect the test results.
If questioned by the regulatory authority, one can point back to the risk assessment performed in the original filing and scientific justification to institute the set of tests already performed. Of course, one needs to be confident in that risk assessment and the justification for why the testing performed in the original filing is adequate. Manufacturers of already commercialized products could justify compliance with USP <382> requirements if the ISO methods detailed in USP <1382> were used prior to the chapter becoming official. The same would be true if alternate testing strategies were employed as long as those methods are equivalent and were validated at the time of use, as detailed in USP General Notice 6.30. Where compliance gaps are identified, the appropriate testing must be performed to meet the requirements of the chapter.
The analytical services and regulatory affairs groups at West can help drug manufacturers navigate the requirements being imposed by USP <382> and perform the necessary testing to assure that products are compliant with the latest regulations. Meanwhile, West’s Technical Customer Support group can help drug manufacturers select the best packaging system for their product, including using West’s DeltaCube™ modelling platform to optimize vial, stopper and seal fit.
Contact us to learn more about how West can help you with your USP <382> testing needs before the December 1, 2025 deadline.
DeltaCube is a trademark of West Pharmaceutical Services, Inc.
i. USP <382> Elastomeric Component Functional Suitability in Parenteral Product Packaging/Delivery Systems; United States Pharmacopeia
ii. USP <381> Elastomeric Components in Injectable Pharmaceutical Product Packaging/Delivery Systems; United States Pharmacopeia
iii. Title 21 —Food and Drugs; Chapter I —Food and Drug Administration, Department of Health and Human Services, Subchapter H—Medical Devices, Part 820—Quality System Regulation, Subpart C—Design Controls. Available at: https://www.ecfr.gov/current/title-21/chapter-I/subchapter-H/part-820/subpart-C/section-820.30
iv. International Organization for Standardization. (2016) Medical devices — Quality management systems — Requirements for regulatory purposes. (ISO Standard No. 13485:2016). Available at: https://www.iso.org/standard/59752.html
v. ICH. Quality Risk Management. ICH Q9. November 9, 2005. Available at: https://database.ich.org/sites/default/files/Q9%20Guideline.pdf
vi. USP <1382> Assessment of Elastomeric Component Functional Suitability in Parenteral Product Packaging/Delivery Systems; United States Pharmacopeia
vii. Title 21 —Food and Drugs; Chapter I —Food and Drug Administration, Department of Health and Human Services, Subchapter C—General, Part 211—Current good manufacturing practice for finished pharmaceuticals, Subpart 94 - Drug product containers and closures. Available at: https://www.ecfr.gov/current/title-21/section-211.94
viii. USP General Notice 6.30 Alternative and Harmonized Methods and Procedures; United States Pharmacopeia. Available at: https://www.uspnf.com/sites/default/files/usp_pdf/EN/USPNF/revisions/gn-rb.pdf



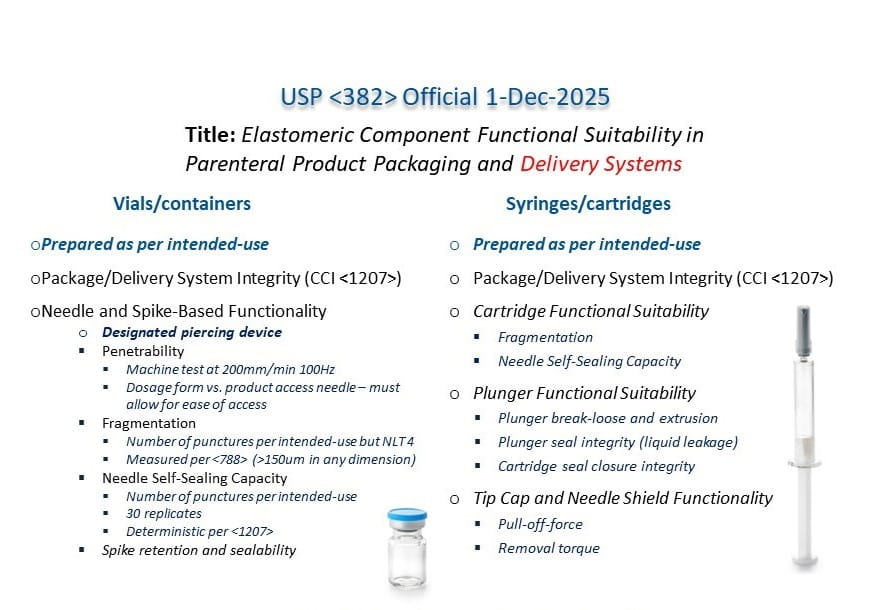 Figure 1 - Summary chart of USP <382> tests for vials, syringes and cartridges.
Figure 1 - Summary chart of USP <382> tests for vials, syringes and cartridges.